Turn your unit into a magnet
for aligned physicians
Map what matters in 12 minutes, benchmark against peers, and publish a Unit Brief physicians trust.


Today’s hiring is noisy and misaligned
Even the best medical directors can't fix what they can't see. Recruiting is noisy. Fit is misjudged. And alignment issues don't show up until after the hire.
Misalignment hurts care
Vacancies stay open longer, and your team's morale drops.
Our solution: Publish a Unit Brief with details candidates are seeking.
Leaders lack visibility
You don't know what's driving disengagement until it's too late.
Our solution: Leader vs. Team Gap score with specific drivers.
No benchmarks, no fix
You can’t tune what you can’t measure.
Our solution: Percentiles by comparable units, plus 3–5 actions.
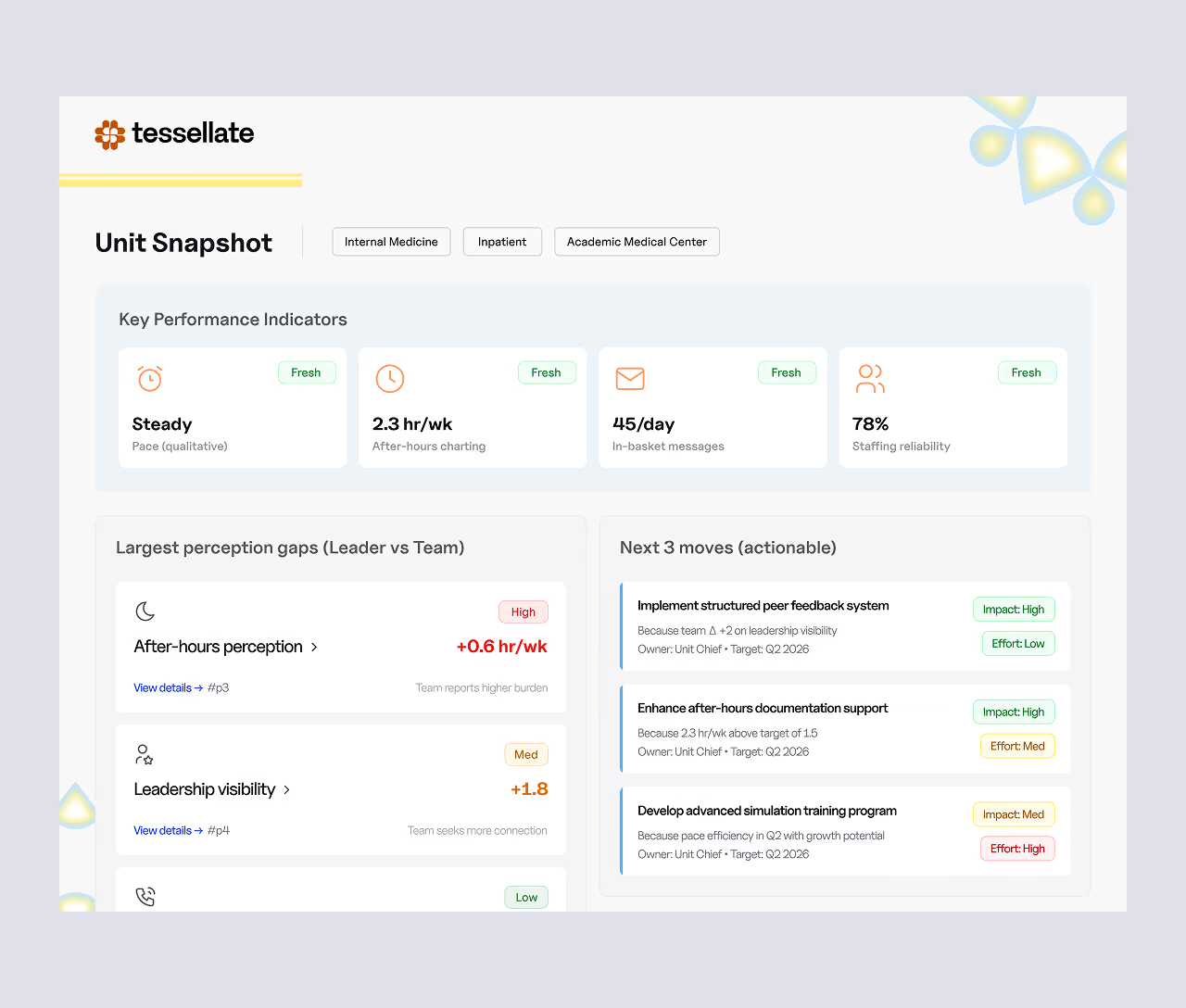
Deliverables you can use immediately
Deliverables you can use immediately
Peer benchmarks
(25th / 50th / 75th percentiles) by comparable units.
3–5 recommended actions
With language you can publish
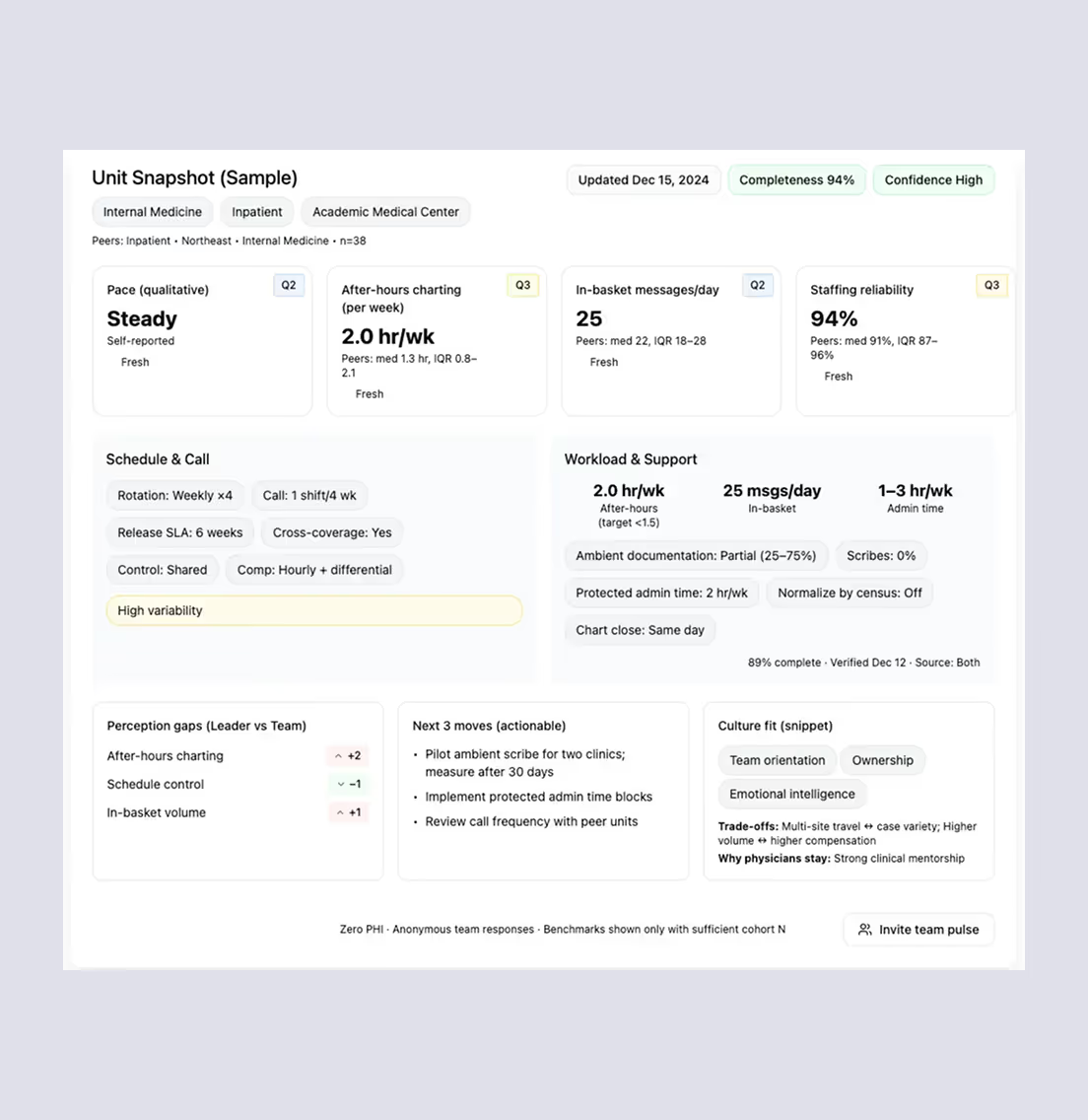
Candidate‑ready Unit Brief
(1‑pager) you can share or use in Tessellate intros.
Invite your team to validate & identify gaps
Include physicians, APPs, and nurses. Share an anonymous pulse to confirm the leader view, surface blind spots, and build trust.
Minimum N=3 for anonymity; we show only aggregates. No PHI collected; opt-out & deletion available.
A fast, evidence-based profile of your unit
Step 1

Survey
(12-15 minutes)
Define schedule, call, workload, support, culture, growth.
Step 2

Benchmark
We cohort against comparable units and score gaps.
Step 3

Invite your team
(MDs, APPs, and nurses)
Anonymous pulse validates reality.
Step 4

Alignment plan
You get top fixes + candidate-ready unit brief

Give your team a voice anonymously
Invite physicians, APPs, and nurses to validate the day-to-day. You’ll see where perceptions differ, what to publish now, and what to fix next.

Anonymous by default
No PHI, min N≥3, only aggregates shown.
Low lift
12 minutes; mobile‑friendly.
Actionable
Gap drivers roll directly into your 3–5 recommended actions.
Six domains physicians screen for beyond title and pay
Team pulse
Parallel perception items.
Rule: show Leader-Team gap only when ≥3 team responses.
Method, cohorting, and privacy
Cohorting
We compare by setting, size, acuity, shift model, EMR, and region to keep it apples‑to‑apples. Minimum N before any percentile is shown.
Privacy
No PHI; team responses are anonymous; opt‑out & deletion supported.

Scoring
5‑point items; we compute percentiles, gap scores, and an Alignment Index (0–100).
Use of data
Aggregated & de‑identified for benchmarks; never sold.
Turn alignment into faster, better hires
Vacancies won't fix themselves. Take the 12-minute survey to see how your team's reality aligns with yours — and attract physicians who stay.



Skeptic’s FAQ
How does the alignment survey work?
It’s a 12‑15-minute leader survey covering schedule, call, staffing/support, workload/tools, culture/safety, growth, and terms. We benchmark your answers against comparable units and generate a Unit Brief plus 3–5 recommended actions. Invite your team to take an anonymous pulse to validate reality. No PHI is collected.
Who should complete it, and can my team weigh in?
The unit leader completes the 12‑min survey. We recommend 3–10 of your physicians, APPs, and nurses. We show Leader‑vs‑Team gaps only when there are at least 3 team responses (to preserve anonymity).
Who can see our unit’s profile?
Only credential‑verified physicians who match your criteria. We don’t post your profile publicly. Recruiters at your organization can view it if you invite them.
What do physicians actually see?
A candidate‑ready Unit Brief—the concrete details they screen for: schedule model & release cadence, call expectations, support ratios (scribes/APPs/RNs/tech), EMR realities, culture markers, growth/teaching options, and compensation structure at the level you choose to share.
How is my data protected?
No PHI collected. Data is encrypted in transit and at rest, access‑controlled, and used only to benchmark and match. Deletion on request and opt‑out are supported.
How does this speed up hiring?
Clarity reduces churn. With an accurate Unit Brief, physicians self‑select in/out before calls. We run consent‑first, packet‑complete intros (pre‑filled applications, documents, interview coordination), which cuts admin and shortens time‑to‑yes.
Do you replace our in‑house recruiters or agencies?
We complement them. Your team stops chasing missing details and unqualified applicants. We deliver aligned, interested physicians with packet‑complete intros so recruiters spend time on interviews, not inbox triage.
How quickly will we see matched candidates?
After your Unit Brief is approved and you enable sharing, many orgs begin seeing aligned interest within 1–2 weeks. Timing varies by specialty, location, and call model; we’ll tell you what to expect for your cohort.
Can we revise or withdraw our unit profile?
Yes. You control what’s shared and when. You can pause sharing, edit details, or request deletion at any time.
Who should complete it?
Leaders start the base profile. Then invite physicians, APPs, and nurses for the anonymous pulse. We only show gaps with a minimum N≥3.
What do physicians actually see?
A Unit Brief with the realities they care about—schedule, call, support, workload, autonomy—no PHI and no names. It’s only shown to credential‑verified physicians whose preferences align with your setting.
Why we exist
We're redefining how physicians and healthcare organizations find alignment — replacing noise and job-board clutter with verified data, privacy, and shared trust.
Because when physicians thrive, healthcare heals itself.